Abstract
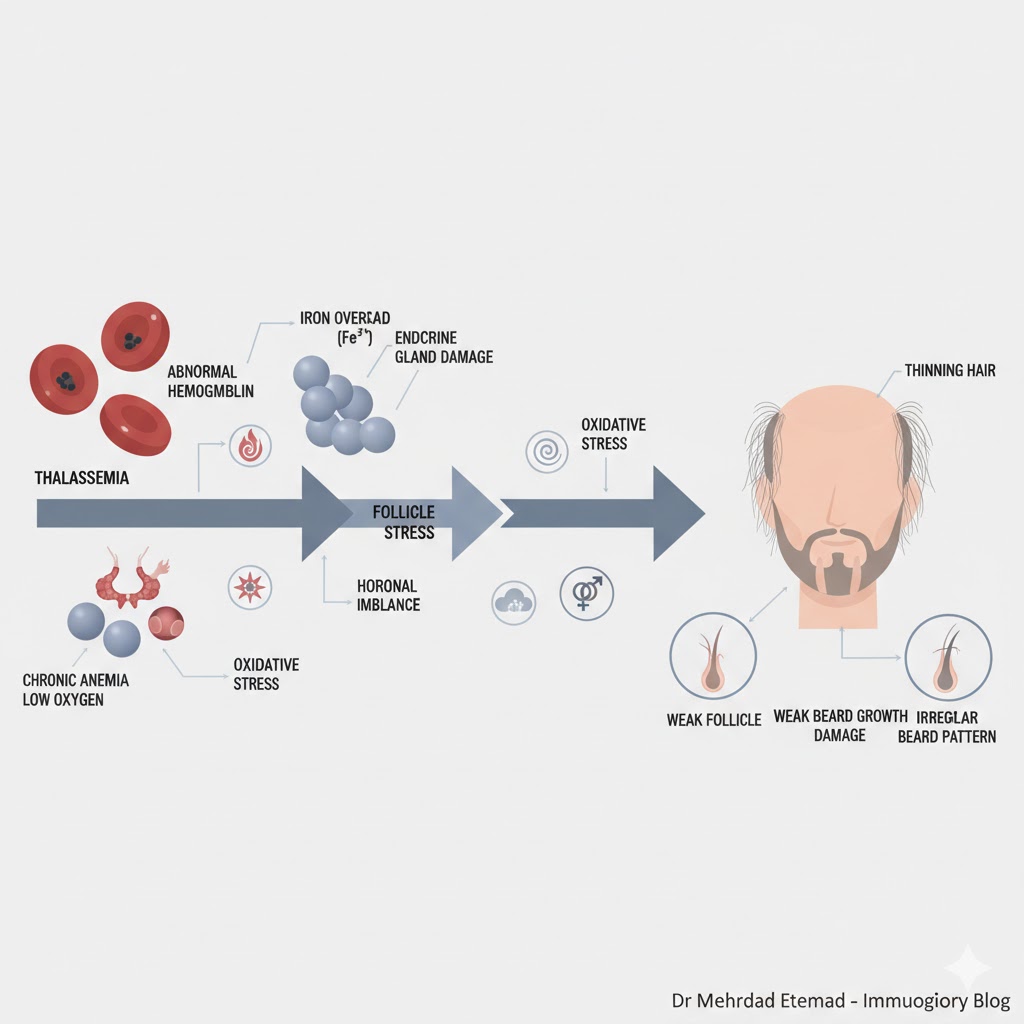
Thalassemia (particularly transfusion-dependent beta-thalassemia) can affect hair and beard health in several ways, ranging from diffuse hair loss and thinning to irregular or weak beard growth. These effects result from a combination of chronic anemia, iron overload, endocrine complications secondary to iron deposition, nutritional deficiencies, and, in some cases, side effects of treatment. Addressing the underlying cause along with topical/systemic therapies and, in selected cases, hair transplantation under specific medical conditions can be beneficial. (References and details provided in the text.)
PMC+1
Brief Overview: Types of Thalassemia
- Alpha-thalassemia: Deletions or mutations in alpha-globin genes — spectrum ranges from silent carriers (trait) to hydrops fetalis.
- Beta-thalassemia: Includes major (transfusion-dependent / TDT), intermedia, and minor (carrier).
- Clinical relevance: The severity of the disease (e.g., frequency of transfusions) determines the risk of secondary complications such as iron overload and subsequent endocrine/systemic effects.
NCBI+1
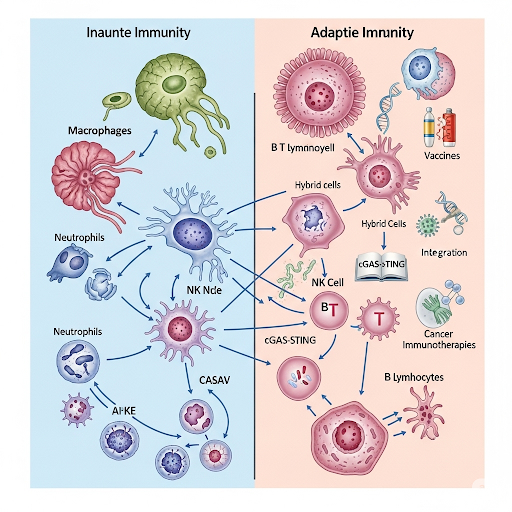
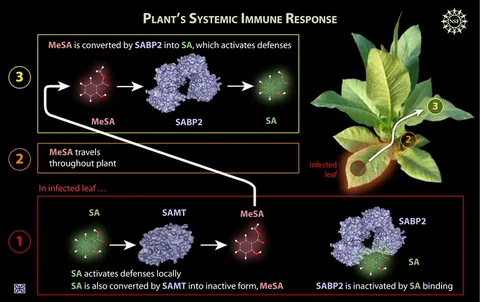
Why Can Thalassemia Cause Hair Loss or Poor Beard Growth? (Mechanisms)
- Chronic anemia and metabolic stress: Reduced peripheral oxygenation may slow down hair growth and shift follicles into the telogen (resting) phase.
- Iron overload: Repeated transfusions lead to iron deposition in tissues, causing cellular damage and oxidative stress — these mechanisms can impair the skin, hair follicles, and endocrine-hormonal axes.
- Endocrine disorders: Iron deposition in the pituitary and gonadal glands can lead to hypogonadism or thyroid dysfunction, both linked to hair loss and irregular beard/hair growth. Studies show high prevalence of sexual dysfunction, delayed puberty, and related endocrine abnormalities in TDT patients.
- Nutritional and metabolic deficiencies: Zinc, vitamin D, protein, or other micronutrient deficiencies may coexist and impair hair growth.
- Drug or treatment-related effects: Certain chelation therapies or chronic infections may contribute.
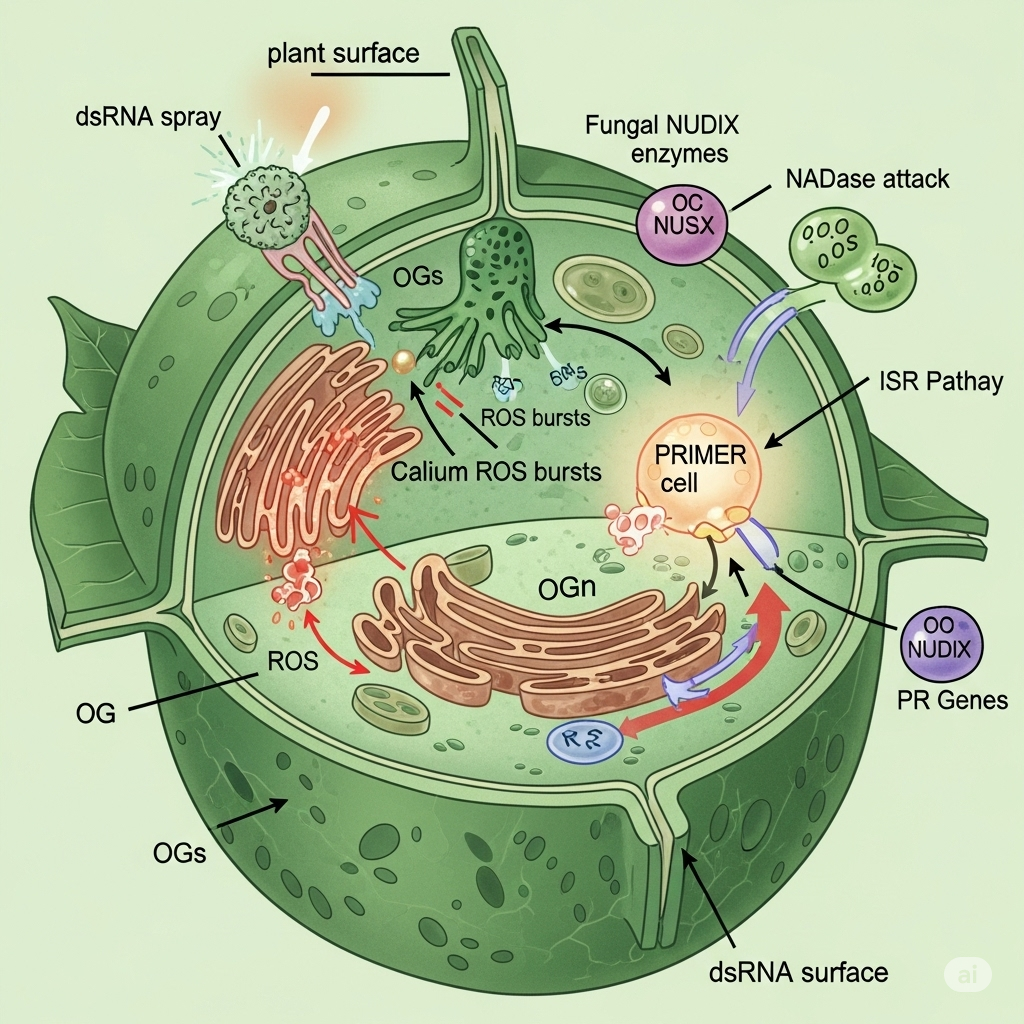
- Chronic inflammation and oxidative stress: Persistent inflammatory states can disrupt follicular cycling.
Summary: The dominant pathway is iron overload → endocrine damage → hormonal/nutritional imbalance → hair loss/weak growth.
MDPI+1
Common Clinical Manifestations in Thalassemia Patients (Hair-Related)
- Diffuse hair thinning, especially during adolescence and adulthood in patients with high iron load.
- Patchy or thin beard growth in males (often due to hypogonadism or low testosterone).
- Alopecia patterns secondary to nutritional or drug-induced causes.
Accurate diagnosis requires dermatological examination, evaluation of hair loss patterns, and laboratory investigations.
PMC
Medical Evaluation (Recommended Laboratory Tests)
- Complete blood count (CBC) – to assess anemia.
- Ferritin, TIBC, NTBI/LIC – to evaluate iron overload (ferritin alone is not sufficient but is a first-line marker).
- Endocrine panel: FSH, LH, testosterone (in males), TSH, Free T4, and diabetes profile if indicated.
- Micronutrient assessment: Zinc, vitamin D, and serum iron (may vary in carriers).
- Specialized evaluations: Hematology consultation and, when needed, liver/heart MRI for iron concentration (LIC, cardiac MRI T2*).
Identifying and treating the underlying cause (e.g., treatable hypogonadism) is the key step, as many solutions stem from there.
General and Specific Treatments for Hair/Beard Problems in Thalassemia
A) Etiology-focused treatment (top priority)
- Iron overload management: Optimize transfusion schedules and chelation therapy (deferasirox, desferrioxamine, etc.) to prevent or slow endocrine complications. Controlling iron overload is essential to reduce secondary damage.
- Endocrine therapy: In confirmed hypogonadism, hormone replacement (e.g., testosterone in males or thyroid hormone management) can help restore hair and beard growth. Requires close cooperation between hematology and endocrinology.
B) Nutritional and supportive therapy
- Correct deficiencies in zinc, vitamin D, and other micronutrients. (Iron supplementation should be avoided unless medically justified, as iron overload is common in thalassemia.)
- Maintain a protein-rich diet and consider supplementation as needed.
C) Topical/pharmacologic treatments for hair growth
- Topical minoxidil: Effective for diffuse thinning (though does not address the underlying cause).
- Finasteride: In androgenic alopecia, for men only and with caution after full assessment.
- Scalp care: Gentle washing and avoidance of mechanical stress.
D) Surgical/interventional treatments (Hair transplantation)
Detailed in the next section.
Hair Transplantation in Thalassemia — Risks, Benefits, and Safety Criteria
Is thalassemia a contraindication to hair transplantation?
Generally, thalassemia is not an absolute contraindication, but thorough evaluation by a hematologist and hair transplant surgeon is mandatory.
Potential issues to assess:
- Hemoglobin level and anesthesia tolerance: Severe anemia may increase anesthesia risk — Hb should be optimized preoperatively.
- Bleeding or coagulation disorders: Platelet count and coagulation profile must be checked.
- Infection and wound healing: Chronic infections or iron overload may impair healing; infection control is essential.
- Endocrine status: Untreated hypogonadism or hormonal disorders may limit cosmetic results.
- Chelation or other medications: Review possible drug–anesthetic/antibiotic interactions.
- Donor site healing: Must be evaluated in patients with poor regenerative capacity.
Benefits (for well-selected patients):
- Restoration of hair/beard density where viable donor follicles exist.
- Improved self-esteem and quality of life — only after systemic stability and safety optimization.
Pre-transplant checklist:
- Hematology clearance (Hb, platelets, coagulation, ferritin/LIC, transfusion and chelation plan).
- Endocrine evaluation (thyroid and sex hormones).
- Infection control (skin/systemic).
- Joint planning between surgeon and hematologist; transfusion or medication adjustment may be needed pre-op.
Dermatoloji Dergisi+1
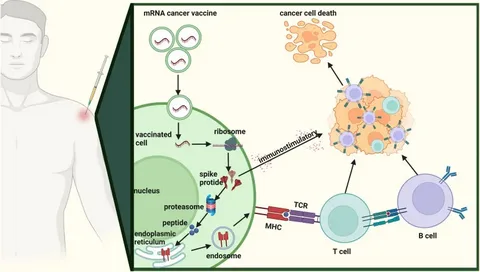
Emerging and Advanced Therapies Indirectly Improving Hair Health
Recent advances in stem cell and gene therapy for beta-thalassemia have shown promising results, reducing transfusion dependency and long-term iron overload, thereby indirectly improving hair and beard health.
Examples include exa-cel / Casgevy (exagamglogene autotemcel), FDA-approved in January 2024 for transfusion-dependent beta-thalassemia, and beti-cel / Zynteglo from earlier generations — both of which significantly reduce iron overload and endocrine complications over time.
hematology.org+2, Çocuk Hastanesi+2
Practical Recommendations — Simplified Algorithm for Physicians/Patients
- Comprehensive clinical evaluation (hematology, endocrinology, nutrition).
- If iron overload or suboptimal chelation: improve management or refer to a specialized center. TIF
- If hypogonadism/hormonal deficiency: initiate hormone replacement under endocrinologist supervision.
- Nutritional support and topical/scalp therapy (minoxidil, care routine).
- For hair transplant candidates: perform full risk–benefit assessment and coordinate timing between hematology and surgery teams.
Dermatoloji Dergisi
Notes for Immunology Readers (and SEO Optimization)
- As an immunology expert, emphasize the relationship between oxidative stress, systemic inflammation, and follicular health — this mechanistic insight strengthens the scientific depth and SEO relevance of the article.
- Highlight the multidisciplinary approach (hematology, endocrinology, dermatology, reconstructive surgery) in management.
Nature
Key References (For Further Reading)
- De Sanctis V. Growth and endocrine disorders in thalassemia. (Comprehensive review on endocrine dysfunctions in thalassemia). PMC
- Evangelidis P. Endocrinopathies in Hemoglobinopathies (2023 review on iron overload and oxidative stress). MDPI
- Thalassemia International Federation (TIF) Guidelines for TDT management.
- Casgevy / Exagamglogene Autotemcel gene therapy updates and FDA approval (Jan 2024). hematology.org+1
- Clinical Reviews (2024): Pathophysiology and novel therapies in beta-thalassemia. MDPI